A recent article by Pauline Chen, MD in the New York Times discusses changes in the medical studies curriculum which are meant to ensure that medical students retain their empathy. Unfortunately the process can and will become undermined by a vicious residency training system. I found that it wasn't medical school that made me cynical. It was a general surgical residency where I was working every other night on call, over 120 hours a week. Didn't know there were 120 hours in a week? Well, I didn't either until I did the math. This translates into up at 5 am, at the hospital from 6 am, then overnight until the next evening at 10 pm, then home for a few hours of shut-eye before you repeat. No wonder I quit my surgical residency after only 6 months!
During that time I was distressed at how I was expected, even encouraged, to continue to care for patients despite overwhelming exhaustion. When I collapsed from the stress I was told that this was somehow my problem, and not the result of my grueling schedule. When I went to a therapist, the situation was normalized and I was prescribed Paxil to deal with my depression and anxiety, when I should have been told to leave. The entire medical education system, I soon realized, was set up to get the most amount of labor from the youngest, and financial incentives existed to maintain the status quo. Residents are essentially an itinerant work force: residents are only trainees from between 3 to 7 years and then they move on. Unionization is nonexistent, or discouraged, and most trainees feel that putting up with the crazy hours is the way to pay their dues and the payoff will come later, in the salaries and perks that come with being an attending surgeon.
I genuinely don't think the system will ever change unless there is some pressure from the outside (i.e. federal regulation) to reform it. The doctors and hospitals who currently benefit from the cheap labor of residents in teaching hospitals have no incentive to change it and the residents are powerless to.
While I admire those educators at Harvard who are willing to invest in improving medical school experiences for their third-year students, they really need to take a look at their own backyard first and first examine their residency training programs. Start with Harvard. That was the where the surgery program I quit 10 years ago was. I wonder if it has changed...
skip to main |
skip to sidebar


Dr. Judy Melinek, a board-certified forensic pathologist and author blogs about forensic pathology and science in the news.
About Me
- Dr. Judy Melinek
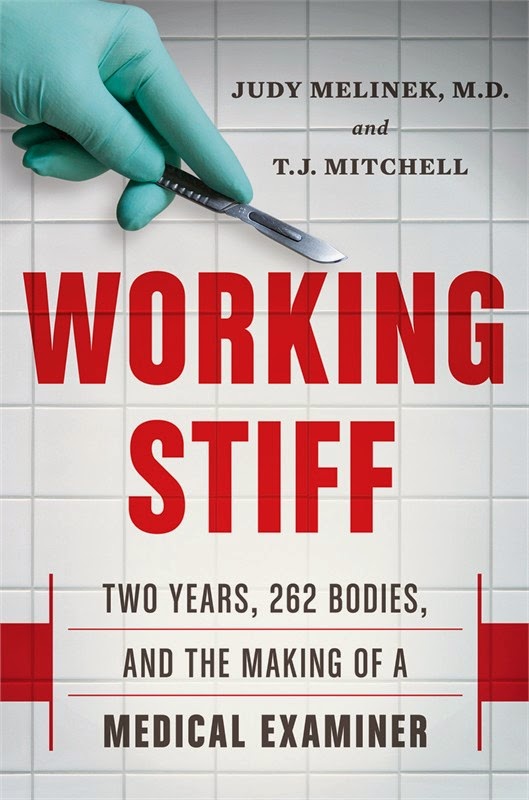
- Dr. Melinek is a ABP board-certified forensic pathologist practicing forensic medicine in Alameda county and San Francisco, California and CEO of PathologyExpert Inc. Dr. Melinek trained as a forensic pathologist at the New York City Medical Examiner's Office from 2001-2003, which is the subject of her memoir, co-authored with T.J. Mitchell, "Working Stiff: Two Years, 262 Bodies, and the Making of a Medical Examiner." She has consulted and testified in criminal and civil cases in New York, Pennsylvania, Florida, Texas, Oregon and California. Dr. Melinek has been qualified as an expert witness in forensic pathology, neuropathology and wound interpretation. She has had subspecialty training in surgery and has published and consulted on cases of medical errors and therapeutic complications. She trains doctors on forensic pathology, proper death reporting and certification.
Popular Posts
-
One of the most common questions I get is "What advice do you have for me if I want to become a forensic pathologist?" These are ...
-
1. Many reviews and press events about Working Stiff list Judy Melinek as the sole author, even though the book is co-authored by T.J. Mit...
-
This article was originally published in Forensic Magazine . To read the original article click here ( http://www.forensicmag.com/articles/...
-
I sometimes get e-mail from high school and college students asking to interview me about what I do. Here are my answers to some of their fr...
-
It was one of the toughest phone conversations I have made in my 15 years as a forensic pathologist. I had just completed the autopsy of...
-
The CSI effect is a term coined by attorneys for the unrealistic expectations created by television crime shows on the public. It's a ...
-
Since the publication last year of my New York Times bestselling book Working Stiff: Two Years, 262 Bodies, and the Making of a Medical E...
-
Originally published in MedPage Today August 16, 2018 (https://www.medpagetoday.com/psychiatry/depression/74589) “My father killed hims...
-
By A.J. Chapman In the 1970s, “The Six‐Million‐Dollar Man” was a popular television show. It concerned a man who had met with a disaste...
-
This article was originally published in Forensic Magazine . To read the original article click here. When a breaking news case involve...
Powered by Blogger.

Copyright ©
Forensic Pathology Forum.
This template is sponsored by Class hits Radio along with Things to do in Jacksonville, Company headquarter phone and penny stock alerts